|
When we consider the current challenges and approaches in Health and Care the reasons to “Take it Teal” become self-evident. The challenges are big and complex and making what we already do more efficient will not help. Indeed, there is evidence that some of these previous initiatives have been counterproductive and have disengaged staff and left citizens dissatisfied with the service they received. The programme to develop Integrated Care Organisations is already underway. Based on subsidiarity, there is no central blueprint, local health and care systems are designing what can improve health in their own neighbourhoods and across their own systems. Moving towards self-organising systems and self-managed teams requires a similar approach. There is learning and experience that can be shared but each system and organisation will need to make it their own. It makes sense to align subsidiarity in the systems and neighbourhoods with subsidiarity in the services that support these neighbourhoods to give them the agility to meet local needs. Health care used to provide treatment for episodes of illness. Its task was to fix the problem and discharge people back to their usual lives. It now needs to deliver long-term support to growing numbers of older people and those living with long-term conditions. This means enabling self-care and self-management of long-term conditions. To be successful health staff need to focus on what’s important to the citizen they are supporting and provide person-centred care. The educational, coaching and developmental techniques used to support citizens to step up and take control of their health and wellbeing are the same approaches that can support staff to take control and manage their own work. Working in this way restores the autonomy removed from workers in recent times and gives them back the ability to make a difference. The improved job satisfaction and customer satisfaction which results improves recruitment and retention rates, another key issue in today’s health sector. Our current approach to health, treating our illnesses and conditions, is not sustainable. We need to work upstream, promote wellness and prevent illness. Health is social, there is a physical element to this and a great contribution that medicine can make but we need a broader appreciation of what makes us healthy and feel happy and well. We recognise that our neighbourhoods and communities play a vital role and we are developing towards being able to value them and work in ways that respect this. In organisations we know that the culture in which we work has a dramatic impact on our performance and our staff wellbeing. Creating organisations and working in ways that maximise the health and wellbeing of our staff and respect and value our communities is a moral imperative. These new ways of working enable us to do this. In health care we are now more accepting of the emotional and spiritual aspects of health, we can prove the benefits of compassion and more holistic approaches to care with patient outcome data. It therefore makes sense that we should view wellbeing and wholeness for our staff in the same way. Creating workplaces where we welcome the whole person allows us to address issues of equality and diversity in context, not as a separate issue. It allows us to value and harness all the talents and passions of our staff to their work, not just the slither of person that might be reflected in a job description. It enables us to model health promoting approaches for other organisations in our systems and treat our staff in the way we hope they will treat the citizens they support and care for. Safety, quality and continuous improvement have long been a focus of healthcare with varied success. Self-organising approaches release the energy of staff and teams committed to doing their best for the people they care for. These staff are best placed to spot the dangers, experience the frustrations and identify the improvements that will deliver the biggest advantages for the people they support. Continuous improvement is an integral part of the self-management team approach. Adopting self-organising approaches in teams and supporting them to pursue their own improvement agenda rigorously will produce the safety and quality we aspire to. Adopting this approach allows organisations to align their operating process with their approach to delivering to their purpose and providing care and support to improve the health of their communities. Whether we look at NHS values, the 6 Cs or the 7 principles of care, this way of working enables us to live them. If we are serious about preserving these values and principles and creating a way for them to not only to survive but thrive into the next 70 years, this is the way forward. Some new organisations are set up with the intention of being self-organising but for many the challenge is a different one. The way an organisation that exists within a traditional management and hierarchical structure can reinvent itself is a focus of Laloux’s current work. This is the reality of most organisations in health and social care. How can it be possible to take a traditional health and social care organisation and move it towards being a self-organising entity? As the Reinventing Organisations movement emerged four years ago, I remember conversations with leaders of new self-managing organisations in the private sector who told me it was quite impossible. They were wrong.
Self-management is the aspect of this new way of working most focused on. The reports of significant savings in the costs of corporate functions, coupled with the ability to re-engage staff through autonomy and improving the quality of services provided, are very attractive. In the health and care world, which traditionally values doing, there is a temptation to focus on re-organising and how we “do” self-management. Ignoring the other elements that make this approach successful, the culture we create, our purpose, the values and beliefs we hold and how it feels to work or receive services are a vital part of this approach and must demand our equal attention. There are various possibilities when considering a transition to this way of working. Some organisations create teams to pilot this method, working as part of but distinct from the larger organisation. To protect this new way of working many projects build a firewall between the pilots and the existing organisation. All communications and interactions are channelled to the new team via a small group of staff and the workload and resources of the team are protected from processes that are used in the wider organisation. It is not yet clear if this approach can successfully transition the host organisations to a new way of working. Indeed, in several organisations hosting these pilots, it is not clear that the organisation itself intends to make this move. There are examples in private industry, perhaps Zappos being the most famous, where leadership has taken the decision to move the whole organisation in this direction and issued an ultimatum. For health and care organisations, who need to ensure safe continuous service, this is not a practical option. Customers may be inconvenienced by lack of new shoes but people and communities would suffer if health and care services are badly disrupted. This adds a whole new dimension to the challenge of change. There are several examples where action by staff groups and communities have halted or seriously disrupted change initiatives in health and care and organisations. Organisations making this move need to be mindful but not paralysed by this awareness. An alternative approach is to work with a whole organisation and support it to evolve in this direction. Some organisations may dismiss this as too complex, too risky and too slow. Indeed, it is not a journey that should be embarked upon without significant consideration, energy and courage. Perhaps because of this, I believe this approach is more likely to deliver successful and sustainable results. When working in the field there is often a request to supply a route map or a project plan to “roll-out” the approach. People want a set of instructions, that if followed will get the organisation to where it wants to be. Herein lies another challenge. This methodology is founded on the belief that rigid long-term plans are not helpful in the VUCA world our health and care organisations inhabit. Every organisation must be alive to its purpose and constantly responding to the needs of the people and communities it serves. The route followed by one organisation, or even a service area in a large health and care organisation, will be different from another. It needs to be, or the organisation will not be taking full advantage of the intelligence, talent and passion of its frontline and the communities it works with. There is no one route map and organisations should beware of anyone that tells them there is. On the other hand, there is a growing and generous community of health and care organisations who already work in this way. They generate learning and advice that can be taken and built upon. From this we can identify some useful foundation stones on which we can base our work. (Read more about these in part 2). We can use this learning intelligently and intentionally to evolve an organisation. Using methods that align with the self-management approach is important in achieving the cultural shift needed for the work. Used skilfully it can provide the pace and assurance of usual project infrastructure and will provide more successful and sustainable results. When we step back, this method is not so different from the work being done to create Integrated Care Organisations. There is no blueprint for this either but a commitment to move in this direction, courage and a willingness to learn together is driving this forward. The content of the work and way the principles are woven together in the new way of working may be new, but health and care has been evolving new approaches, breaking new ground and achieving the impossible for decades. It’s time to rediscover those abilities. The 7 Most Common Myths and Misunderstandings about Self-organising in Health and Social Care15/7/2018
1. Self-management means no managementIn traditional organisations the tasks of decision making, providing expert clinical advice, allocating work and resources and monitoring and assuring the work being done are often all part of the managers role. In a self-organising team these tasks still exist but are done in a different way. Teams that work successfully adopt processes to help them manage themselves and hold each other accountable. The process of peers holding each other to account about their practices and efficiency can be much more powerful and effective than traditional management methods. Common techniques teams use to help them do this are tactical meetings, integrated decision making, regular consideration of statistics and stories that enable the team to know where they are at and plans to continuously improve.
2. There is no hierarchy There is no power hierarchy, no-one is given power over their team mate. Natural hierarchies do arise and are encouraged by building an environment that welcomes the whole person to work. Someone who is considered efficient and fair is an obvious choice to fill the role of organising the rota or can be the “expert” that supports others who want to develop the skills and aptitudes for this task. Similarly, a colleague who is an expert in a clinical aspect of work will naturally take a lead in discussions and developing practice in this area. She may even find she is asked for advice and input by other teams. 3. Teams are left alone to get in with it Teams are supported to self-organise by coaches or facilitators. Coaches and facilitators have no power in the team. Their role is to provide advice, information and support the team to make decisions and resolve issues. Depending on the type of team or organisation, some teams are also supported by business managers who handle contracts on their behalf or carry out other specialist functions. 4. Teams act independently and do as they please Teams taking decisions often use integrated decision making and the advice process. This ensures that they take advice from any experts and talk to anyone who may be impacted on by their decisions. The decision is the teams to make but they will be taking the decision having integrated any views and objections they encountered. Teams may also link with other teams to consider issues they have in common. For example, teams may send representatives to a meeting that they have empowered to make decisions about staff training. The meeting would be accountable for planning the programme and spending the budget on behalf of all the teams. Systems and processes based on holocracy or sociocracy are often used to connect teams and their decision making across larger organisations. 5. There is no leadership There is distributed leadership. Many people taking different roles will be required to take decisions as defined by their role, instigate action, resolve problems and monitor quality and outcomes. Especially as an organisation establishes itself or makes the move to become self-organising leadership is key. Leaders need to create the spaces for the self-organising behavior they wish to encourage and keep inviting people to step up and take part. They need to have courage and hold a steady course as the organisation encounters its first problems and setbacks. They need to articulate the purpose and values frequently and clearly so that teams can make decisions and check they are in alignment. Leaders need to create the environment in which the teams can flourish. They need to collect and provide information to teams to make great decisions and to external regulators and stakeholders to assure them that the services provided are safe, effective and compassionate. 6. Only highly skilled senior professional staff can work in this way Anyone in a health or care organisation can work in this way. We already have many of the skills and self-organise in non-work situations all the time. There are examples of the lowest paid, lowest grade staff working successfully together in self-organising teams. There are also examples of the highest paid, highly trained and educated staff who have not been able to work successfully in this environment. The approach is about working as part of a team. Being able to give and receive feedback, being accountable, being supportive, being humble, being proactive in identifying and solving problems and being trusting and trustworthy are all attributes of successful self-organising team colleagues. 7. There is a blueprint about how to do this The teams and organisations working in this way are very generous. Both inside and outside health and social care they will share their experiences and knowledge with you. There are lots of shoulders to stand on to see the way forward for your team or organisation. This way of working is so successful because it enables every individual to contribute their best to their team. Similarly, it enables every team and organisation to offer what is most useful to the people and communities it supports. As a result, each organisation will be different. Indeed, each team made up of different team members and serving a different community in an organisation will be different. The thing that unifies them and serves to measure their success is that they can fulfill the organisations purpose for the people and communities they serve. There is no blueprint but there is a lot of knowledge and experience that you can use to plan your own journey. Jane Pightling www.evolutonaryconnections.co.uk Values based recruitment? Only if you mean it. Values based recruitment is becoming an increasingly popular practice. It’s been around for a while now in health and care and lots of other industries too. Charities such as Skills for Care offer toolkits and support. The NHS offers its own guidance and organisations like NHS Employers offer similar resources and services. It must be a good thing, right? Organisations using these methods report many benefits including improved staff morale, lower sickness and absence rates and better quality of services provided. Skills and knowledge can be developed once someone is in the job. Knowing that a new employee shares the values of the organisation and will fit well into the team culture is surely something worth putting time and resources into.
I think value-based recruitment is an amazing thing. I experience great joy working with organisations to develop and deliver values-based recruitment approaches. There is nothing more satisfying than working with a group of people and being confident that the organisation has got the right person for the job and the person has got the right organisation for them. It’s as much about the person choosing the organisation as the organisation choosing the person. Its wonderful to see people grow and develop in an environment where they can flourish, and I believe values-based recruitment can provide a great start to enable this to happen. As this language and practice becomes more popular I would add a caution. As an organisation and a leader you must really mean it. As an organisation its worth spending time and effort considering your values. Are they relevant? Are they alive in your organisation underpinning the decisions and demonstrated by actions and behaviours? Your values statement must be authentic and as a leader you must live it. The dark side of this practice is recruiting staff to your espoused values and then failing to deliver. In health and care the values we look to align are our core or focus values. These are the ones that when fulfilled provide meaning to our work. Values change depending on our age, experiences and circumstances but some remain more constant and are rooted in our upbringing and culture. These values are the ones that when transgressed are likely to provoke us to shout back at the television, to dislike someone or be extremely angry with them. When someone is recruited on a values basis to an organisation, they believe that they share values. The organisation offers them a vision of a world the person aspires to be part of. They expect to experience their core values in their day to day work. When the organisation fails to deliver this the effects are devastating. As a coach, the people I support to make decisions about career future where core values have been transgressed are the most angry and bereaved. When organisations do not deliver on values-based promises people feel utterly betrayed. This is dreadful for the employee and damaging for the organisation. These people do not forget their experiences and sometimes do not forgive easily. Values based recruitment is amazing if executed sincerely based on authentic values which the organisation is truly committed to. If not, then please don’t use this as the latest marketing tool to attract new staff in a demanding market. The results are cruel and messy.
Thinking about the disengagement many health and care organisations are struggling with at the moment I took the opportunity of a long journey to revisit Brene Brown. She has some useful thoughts. When I think about the cultures of many health and care organisations and the belief and value systems of powerful groups that work within them, there is a discomfort with the spiritual and the emotional. In health care we are beginning to accept the health promoting power of communities and recognise the destructive impact of loneliness and isolation for the people we support and care for. We are much less able to recognise and embrace the potential of emotions and spirituality in our staff and our leaders.
Brene argues that it is vulnerability that is the core of all of our emotions. By walking away from our vulnerability we walk away from emotion which is what brings meaning to our lives and work. Vulnerability, she argues, is what we need to do difficult things well. When we have difficult conversations with our colleagues and the people we support and care for from a place of vulnerability we make real connections, enable new possibilities and make a difference. When we recall instances where we have made a real difference to the lives of our colleagues and the people we support and care for we can often identify how we took the risk and courageously showed up as our real selves. Many organisations are struggling with situations where this courage is lacking. Staff experience a disconnect between their values, often the values they thought they shared with their organisation, and the way they experience their work and organisational leaders. They experience shame, believing they are not good enough and their organisation is not good enough. When staff work for organisations like the NHS, personal pride and identity is often closely tied to the reputation of the organisation they are part of. Being told by public leaders and the media that the organisation is not good enough, that it is failing the people it intends to serve, is a message that has been taken on board personally by many staff. Brene also identifies the impact of comparison and how this can limit our creativity and enforce a very narrow standard that excludes many of us and cannot meet diverse needs. As I think about our preoccupation with comparing ourselves across and within health and care organisations I can see that this is true. Staff who have a deep understanding of what is important to and needed by the people they support are denied the opportunity to create new ways of working and delivering what’s needed as practices and ideas are transplanted from other “more successful” places. So if we revisit Brene and apply what she has to say, what would it be like? We would intentionally create organisations where our emotional and spiritual selves are valued and we are supported to be vulnerable. Places where our courage to be vulnerable and do difficult things with authenticity is recognised and celebrated. Where the need to be perfect is not allowed be the enemy of good. Organisations where we make comparisons to learn not to shame, and to help us consider who we have excluded. Where we can talk about the guilt of making a bad decision or doing the wrong thing from a place of vulnerability not shame so that we can learn and grow. We would create cultures where we can “Dare Greatly”. Where, as Brene would encourage us to do, we consider not what we would do if we couldn’t fail but what’s worth doing even if we do fail?
Inspired by Brene Brown (and airport delays!)
https://www.penguinrandomhouse.com/books/310307/daring-greatly-by-brene-brown/9781592408412/
By Anna Betz and Jane Pightling for Enlivening Edge Magazine Part 1
http://www.enliveningedge.org/views/self-management-save-health-and-care-systems-integral-european-conference/
The role of transformative listening in transforming self and organisations
When both staff and patients have a lot of re-learning to do, we need to develop more advanced skills to listen more deeply to each other, to our own and each others’ values and motivations. We need to learn what it takes to use knowledge wisely to co-create health with individuals and communities. Liberating creative potential encourages the emergence of new insights and practices which is evidenced by the newly formed Wellbeing Teams in the UK. The healing of our broken health and social care systems will require active support of self-care, facilitation of self-knowledge, and working in a highly relational way. This work of healing is inseparable from the way we organise our larger systems of health and care. Courageous and visionary leaders who really care for the system as a whole, and staff who are ready to live their values by working with patients in a way that is empowering, are starting to come together to co-create more dynamic organisational structures. The art of listening is central to this transformative work. Initiatives such as Making Every Contact Count and Shared Decision Making and Health listen to citizens and support them to feel responsible for their own health, and to make lifestyle choices that will enable them to live the life they aspire to lead. This allows them to discover and keep doing what matters to them. If we want to succeed in co-creating healthy systems and health-generating communities, we need to listen from a broader, less outcome-fixated perspective, and create together the conditions that become a fertile soil for the emergence of innovative ideas and practices. Professionals will need to redefine relationships with citizens, and to recognise that we can add value only if we co-produce a solution that recognises the citizen’s strengths, and focuses on what matters to them. Similarly, our organisations need to redefine relationships with our communities. They need to learn to listen without trying to control outcomes, start giving space to communities, and intervene only when invited to help or requested to do things that the community cannot. In this article Anna discussed this aspect in more detail. Jane lives and works in a community that is encouraging staff and citizens to embrace and participate in this new relationship as partners, spending time and resources listening to communities, and developing creative ways to support and provide what the community requests. This has meant developing learning opportunities and coaching for citizens with long-term conditions, co-facilitated by professionals and people with lived experience. It has involved diverting resources to enable citizens to set up groups and networks that meet their own needs. For example, very small resources were required to start an outdoor activity group for dads and children wanting to improve their fitness or to provide a community meeting space for older people with mental health issues to talk and provide each other with support. The setting up of groups and networks included diverting resources to fund a worker to work with homeless people, resisting pressure from the press and local politicians to “remove the problem quickly”. It meant working on the street, listening and waiting until the people themselves decided the time was right to change. It meant supporting the community to come together to develop town centre initiatives to connect existing resources and co-produce and co-implement a plan, securing new resources to provide accommodation and support people back into housing when they are ready. To change the way we have been conditioned by our political, social and educational system to think about healthcare, organise, and deliver it, clearly requires new ways of understanding, designing, and providing it. How can we discover an approach that is energising, revitalising, and enriching, one that builds on strengths and assets within and amongst individuals and communities? It all begins with the quality of our listening and with allowing ourselves to be challenged and transformed by what we sense, hear, and feel called to do and manifest in our lives. Allowing ourselves to be challenged without behaving defensively is connected to a certain quality of thinking or a mindset that we apply when we approach situations. What if the challenges we meet in our life and work are gifts to help us in discovering what else is possible? How can we learn to relate to our own experiences, to each other and to professionals in a way that is empowering and transformational? Otto Scharmer calls the shift in mindset that enables us to connect with more of our human potential a shift in evolving human consciousness from habitual ego-system to eco-system awareness. An eco-system awareness is focusing not only on one’s own wellbeing but on the wellbeing of the whole which broadens the mindset and helps us to listen with more openness. The authors Anna and Jane, along with Helen Sanderson, work in different roles in the health and care sector in the UK. We look forward to sharing with you at the Integral European Conference in May some of our experiences and practices, and we invite you to co-sense and co-discover with us where this journey could take us all. If you are curious about the part you can play in re-inventing health and social care, why not register for the IEC2018 conference and join our two workshops on Friday 25th May? When you register to join the conference following this link don’t forget to mention that you are interested in the Teal Organizations Track.
Join the conversation and help to discover through deep listening what in Christiane Seuhs-Schoeller’s words our “superpowers” are. According to Ria Baeck “most people don’t know and are not aware of what their unique gift to the world is. It is just inside them, totally normal and easy to access.” She has tried to write it in these words: http://www.collectivepresencing.org/6-2-from-authentic-self-to-souls-calling/ To continue the conversation and engage in action together join us at the conference following this linkand remember to mention that you are interested in the Teal Org Track. Part 2 of this article will be published soon. Anna’s background is in Health and Social Care with training in Herbal Medicine, Socialwork, Mindfulness Practice, Transparent Communication, and Systemic Family Therapy. She practices a pro-active evolutionary approach to Health and Wellbeing and leads on projects in the UK National Health Service using Mindfulness and diet for people suffering from chronic inflammatory diseases like diabetes and dementia. Her passion for building thriving and sustainable communities inspired her to co-found the HealthCommonsHub. She feels at home in places where individual, communal, organisational, and social evolution meet, and where people support each other in becoming whole and feel enlivened. The Sustainability and Transformation Planning process challenges health and social care to achieve two huge tasks. Redesign and build a new system around the needs of people and communities and do it in a financially sustainable way. To add to the complexity STPs are caught in tensions between central government and local control, long term aspirations and short term crisis and the recognition of the potential to realise huge change against the scepticism that this is just another way to cut budgets and services. It’s not only the outcomes and environment that are challenging. To succeed the system and the people in it must begin to work in a whole new way. Local leaders have been given joint responsibility to deliver. This demands a refocus from the internal hierarchies and individual organisations to spanning boundaries and building authentic relationships and networks across the landscape. Changing demographics and demands; depleted financial and staff resources; new technology; changing patient, staff and community expectations and redefining of illness, health and well-being all combine to create a complex, unpredictable and sometimes volatile environment for this work.
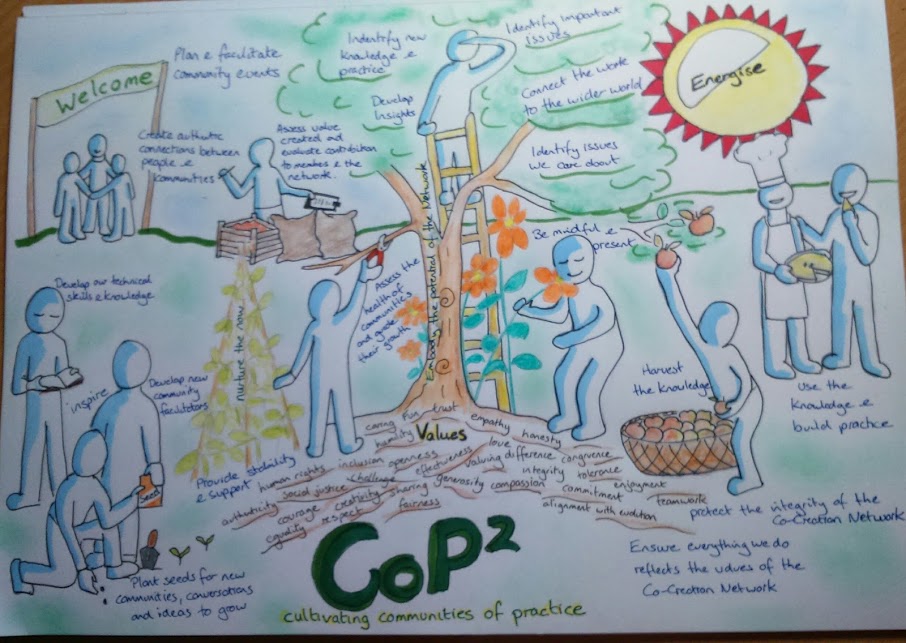
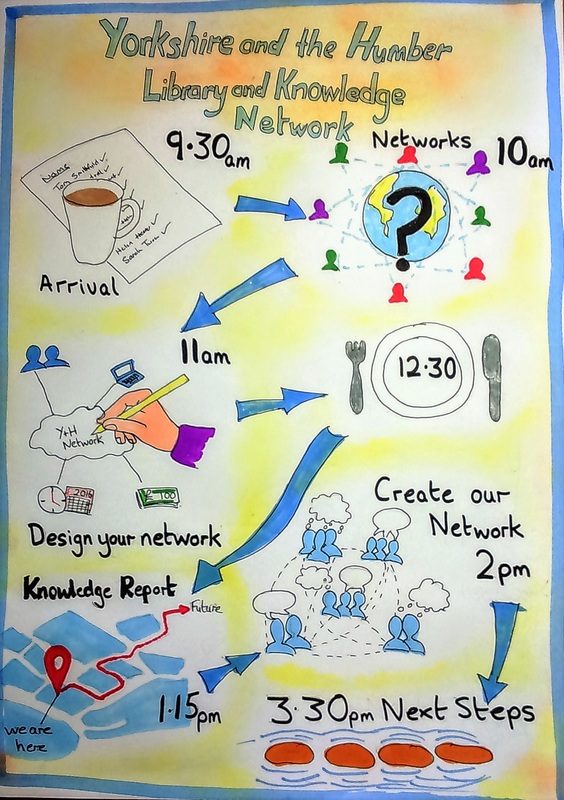
To work well as systems leaders, thinking beyond the usual focus of one organisation and instead holding what benefits the whole system requires relationships built on trust, shared values and the ability to appreciate contributions from all parts of the system. It also requires a huge change of perspective. We need to move from organisation based discussions focused on acute hospital ward closures to apply generative listening to the people and community who need the services and the staff who are passionate about and committed to providing it. When we take a step back and look at this challenge, it is obvious that conventional change management alone cannot deliver. It would not be efficient in terms of use of management staff and resources, or effective in terms of facilitating the innovative and inclusive approach that this task requires. Leaders need to set clear direction, boundary the space with information about standards, available resources and needs and then step back and empower and enable their staff and communities to develop, own and execute the changes. This is an anxiety provoking situation and travelling the road together is always slower than forging ahead as individual organisations or services. So, despite the pressure we must progress at a measured pace if it is to be done sustainably. It is because leaders are now fully appreciating the situation and achieving the confidence to hold the space and step back that Communities of Practice are becoming a popular way of working. Communities of Practice work first to bring people together around a shared interest or domain. This can be a professional or academic interest and can also be about personal or lived experience. Bringing different expert experiences and tacit knowledge together and enabling people to develop shared stories, collective sense making and shared values develops a group identity and relationships where deep learning and new knowledge and practice can be developed. Communities can bring people together across traditional boundaries, encourage groups to identify their most burning questions and facilitate them to co-create new knowledge and practice in response to the most complex challenges. Staff involved in this way of working have reported a reconnection with motivations and values that they felt had been lost in their work. Patients, service users and carers spoke about being heard and valued as their experiences were validated and aspirations recognised. Perhaps most importantly Communities are generating innovative, sustainable solutions to sticky problems and creating real value for themselves, their organisations and communities. Proof perhaps that “None of us is as smart as all of us”. I never imagined that I would be able to provide visuals like this. I was under the impression that you needed to be good at art and drawing. It was a liberating experience to find out that actually it helps not to be too confident and experienced at drawing. This allows us to keep it simple and concentrate on what it is exactly we are trying to communicate, not the drawing itself. With some expert guidance I found I really enjoyed it. There's great pleasure in seeing a project or piece of work communicate its value in such a powerful way. It's been incredibly useful. Many people have a preference for visual communications and in situations where it's vital that everyone can participate, it helps provide inclusive communication. It's also been very popular with groups I didn't expect to like it so much. Busy managers and clinicians appreciate how much can be efficiently communicated in a visual. Thank you Cara and Graphic Change I look forward to learning more.
First published Dec 2015  I remember at a meeting, talking to someone working to establish a Teal organisation who told me that the NHS could never be Teal. The NHS is a long way from Teal, for sure. The NHS as a governmental entity is formed of many different organisations. Right now it’s probably more of a rainbow than any particular colour, in terms of the developmental stages of its units. Even so, the NHS and the services it incorporates have made many big changes previously. For example, I was part of the alliance between health and social care staff, families, and service users that worked to move mental health care out of the asylums and into communities. I have worked with some amazing people and I have seen them do incredible things. Maybe they can evolve a Teal NHS; I think so, and this is why. The Current NHS Customarily, particular NHS services have been keen to police and protect their own borders, responsibilities, and resources. In the worst cases, people are bounced between different services, and struggle to find their way in a complex web of providers and eligibility criteria. Sometimes they fall in-between services and their needs go unmet or they just give up. For example, when I was pregnant I had pregnancy-related carpal tunnel and needed a wrist splint. I was told by the physiotherapist I saw at my local primary care clinic that she couldn’t provide it to me, as her budget didn’t cover pregnant women. She advised I should travel into the city to the acute hospital maternity unit and see the physio there. I gave up and bought one via the internet. Institutional Context of the Co-Creation Network of Communities of Practice I have been working for the past year with a group of NHS clinicians, academics, service users, and staff from charitable and private industry to establish what we call the Co-Creation Network which encompasses a variety of “Communities of Practice” committed to making improvements in the health and social care system. The Teal characteristic of evolutionary purpose is evident in that these Communities are about making improvements partly by breaking down the traditional boundaries of health and social care services, and encouraging/implementing a community-encompassing approach. The Network is sponsored by two regional NHS bodies: Yorkshire & Humber Leadership Academy and Yorkshire & Humber Academic Health Science Network. Both regional bodies recognise that the challenges faced by the health and social care system require something very different. Both bodies have struggled to hold the space for this Network and the different approach it takes, against the usual system demands for performance management to justify any investment and direct activity. Communities of Practice are a voluntary, not delegated endeavour. Some participants are given leave to attend meetings and events in worktime, but most CoP activity is done in members’ own time. Thus, membership in a Community of Practice requires great passion and personal motivation. How the Communities of Practice Operate Each CoP is people working together to co-create new knowledge and practice in an aspect of their own field. Communities are varied, focusing on whatever their members see as important. For example, Communities of Practice have been established to consider Sepsis, Medication Safety, and Creating Caring Cultures. The Sepsis CoP is working on awareness-raising techniques to address an issue that people have not been well aware of previously. The NHS system has given them implicit permission by tasking staff or organisations to reduce sepsis incidents, but has not given directives on how to do this. So the CoP has the freedom to develop and implement some “How’s.” You might be wondering, how do new “ways” get authorized to be implemented and put into practice in various settings? In some cases, the system has not given permission (versus the implied permission re Sepsis concerns) and the CoP may be challenging received wisdom and practice. Some CoP’s have been formed with the express intention of doing such challenging, as they strongly believe that current practice is not good enough. CoP’s looking at changing the traditional relationship between professionals and patients are often in this position. Part of their learning is how to identify and influence key stakeholders to co-create a new approach. The Communities of Practice are courageously pursuing new knowledge and new practices that they believe can bring real value to the services they provide. In an acute hospital, a Community of Practice has introduced mindfulness practices for staff and elderly patients. It is reporting a real cultural shift in the ward environment, and a huge impact on patient safety, with fall rates hugely reduced. This Community is now turning its attention to how it might extend this ethos of care out into the community to involve everyone who might provide support to their patients. A Community of Practice was formed by a group of staff developing a new role in primary care to connect services and provide better care for older people with complex health needs. In the UK, locally-based clinics provide access to doctors, nurses and health care support staff as the first point of contact − and principal point of continuing-care contact − for services dealing with ongoing health conditions. It was noted that an older person with several long term conditions such as heart disease, diabetes, and dementia would be in contact with their local primary care doctor and nurses, but would also have links with a huge variety of other health and care organisations including specialist medical services provided at outpatient clinics in acute hospitals, specialist community-based teams such as mental health and dementia care, specialist home care services from a physiotherapist or occupational therapist, nursing visits from charities, as well as support and care workers from not-for-profit care companies. This Community of Practice is noticing early signs of expected success in reduced admissions to hospital for this patient group as all those services work better together to keep the person safe and well at home. There is also a vast array of other benefits from this CoP’s connecting of services. They include improved understanding and appreciation between different government-provided health and social care services, good relationships between different locally-based clinics, authentic connections between statutory (government-provided) services and community assets and resources, and a commitment from all elements of the whole system to improve the support provided to these elderly members of their local community. Next-Stage Challenges Faced and Dealt with in CoP’s I believe my experience provides one bit of clear evidence that the three Teal principles of self-management, evolutionary purpose, and wholeness have been readily adopted as core principles by some NHS staff and those working with them. I am sure there are other examples too. The Communities of Practice established as part of the Co-Creation Network adopted these principles despite the fact that they were challenging and difficult at first. Self-Management Communities of Practice are self-managing by definition. They set their own agenda, organise themselves, and also decide what learning they will pursue and how they will use this knowledge. This was a shock to many NHS staff involved, and it was difficult not to seek permission and direction from elsewhere. Many of us experienced confusion at first. “What is it we are supposed to do?” Communities moved swiftly from confusion to feelings of liberation and then action. Members gained confidence, established relationships, defined their shared agenda, and organised meetings and “learning expeditions” — our title for the work to answer the questions we have set ourselves. Wholeness One of the most unifying and important aspects of the Co-Creation Network is the way it supports wholeness. The Network adopted mindfulness practices to help stressed, overstretched members be fully present in their Communities of Practice. The opportunity to make authentic connections and pursue work that they identified themselves as important was cathartic. I think it may have even persuaded some members, who were disillusioned and damaged by their working environments, to stay within the NHS and work towards change. “This work gave me space to connect with that passion again and start to explore what could be possible. Through learning about CoP’s I could see that I wouldn’t make it to the top (of the mountain) on my own, but I could take others with me and we could support each other on our difficult journey. And that the journey itself would make us stronger, through sharing and learning together.” Community of Practice Member Evolutionary Purpose Perhaps most inspirational is the evolutionary purpose evident in the Network and its Communities of Practice. Free to pursue their own agendas, Communities of Practice have been established to consider pharmacy, mental health and childbirth, work with older people, the role of mindfulness in healthcare, Innovation, Musculoskeletal Practice, and many other areas. However, it’s not the rich variety of learning and practice being developed that I find so significant; it’s the way this is being done, described in this article. Like for Buurtzorg in the Netherlands, the results can already be termed “outrageous”. (Laloux, 2014 Reinventing Organisations, Chapter 2.2 Outrageous Results paragraph 1) “There was an absence or at least a much reduced sense of fear about “doing it wrong;” this felt different from much of my previous experience of the NHS.” Community of Practice Consultant Reinventing the NHS as Teal Contrary to my own typical experience of “falling through the cracks” of the system, now more new Communities of Practice are focusing on working across traditional service boundaries, and often exploring a geographically-defined approach which reflects the community or neighbourhood experience of the people accessing their services. These Communities of Practice seem to have found a real evolutionary purpose. They are working towards breaking down traditional NHS boundaries and developing new ways of supporting health and well-being in an environment where it is clear that health and social care needs to radically reinvent itself. Maybe the person I met was right after all. The NHS as it is now cannot be a Teal organisation. But the NHS that will be, must evolve to become a Teal organisation. previously published Enlivening Edge 27th October 2015 http://www.enliveningedge.org/organizations/uks-national-health-service-nhs-cannot-teal-organisation/#more-1448
I had an unexpected childhood. In the early 1970s my father left his respectable and secure job in a nationalised industry and headed off to university. It wasn’t until I was going through some of his books after he died and came across a passage he had marked about education for education's sake, that I began to appreciate why he had taken this decision. As a student at Ruskin College Oxford, Ruskin’s concept of education as “leading human souls to what is best, and making what is best out of them.” was a core aspect of his motivation to become an educator. In the 1970s it was not done to leave a good job and pursue an uncertain future, especially if you were already in your thirties with a young family to support. I will never know what made him realise that the steady job would not be steady for much longer or what gave him the courage to pursue what was really important to him. I do know that it delivered financial stability and despite its challenges, I think it delivered real job satisfaction too.
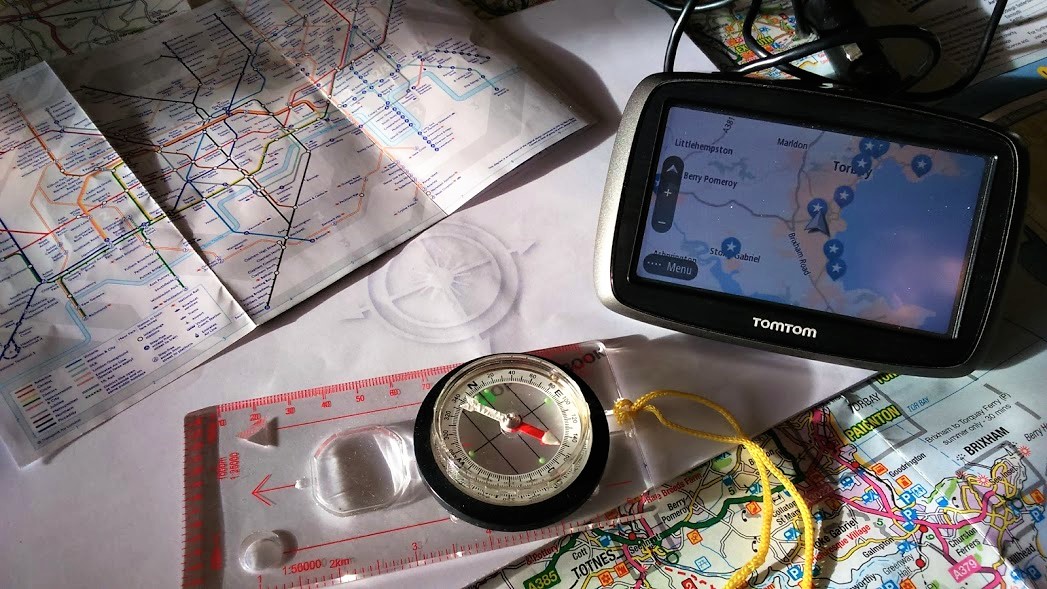
My father’s actions were unusual at the time but now his story seems much more familiar. There are a number of recent pieces of US and UK research recording how most of us will have a number of jobs with an increasing number of employers during our working lives. The Association of Accounting Technicians research in 2015 interviewed 2000 people and found that 46% would change their career completely after finding their current path wasn’t for them. It is much written about that millennials and younger people in the workforce expect much more than a wage packet as fair recompense for their labour. Our relationship with work is more complex and sophisticated than it used to be. Whilst income is important; job satisfaction, well-being, work-life balance, development opportunities and working for an employer that demonstrates social responsibility and where we feel proud to be part of the organisation are also key. It is now recognised that being able to align our personal values and motivations to that of our business or employer is vital to productivity. When we are not fully engaged with our jobs, when we are not convinced our job is worth doing, when we don’t feel we are making the best of our talents, or being enabled to do the best job we can, we are less efficient and the quality of our work suffers. The CMI Quality of Working Life Report 2016 found motivation was becoming an increasing challenge for managers, 28% reported feeling not very motivated or not motivated at all. Over a third of public sector managers reported feeling demotivated and working at less than 70% productivity. More now than ever, it’s important to have a clear understanding of what motivates and drives us and how we can align this in our work to do a job worth doing and do it well. The fast changing world of work and business means that we need to accept that the "what" and "how" of our work will change frequently. We must have a deep understanding of the "why" in order to provide the compass to navigate our future career path and deliver satisfaction, well-being and success. This article was inspired by Lani Morris https://www.greenleaf-publishing.com/the-map-of-meaning |
AuthorJane Pightling has experience across the public, private and charitable sector. Through her work in the NHS Leadership Academy and her consultancy Evolutionary Connections she developed complex systems leadership capacity, providing training, coaching programmes and establishing networks and communities of practice to sustain learning. She maintains her social work registration and her commitment to person centred and community focused approaches. Jane has a deep interest in the potential offered by new ways of working, designing and building organisations and communities that can best deliver this kind of service. She works with organisations and leaders to develop approaches that design in autonomy, wholeness and purpose. Archives
October 2021
Categories
All
|







 RSS Feed
RSS Feed