|
I never imagined that I would be able to provide visuals like this. I was under the impression that you needed to be good at art and drawing. It was a liberating experience to find out that actually it helps not to be too confident and experienced at drawing. This allows us to keep it simple and concentrate on what it is exactly we are trying to communicate, not the drawing itself. With some expert guidance I found I really enjoyed it. There's great pleasure in seeing a project or piece of work communicate its value in such a powerful way. It's been incredibly useful. Many people have a preference for visual communications and in situations where it's vital that everyone can participate, it helps provide inclusive communication. It's also been very popular with groups I didn't expect to like it so much. Busy managers and clinicians appreciate how much can be efficiently communicated in a visual. Thank you Cara and Graphic Change I look forward to learning more.
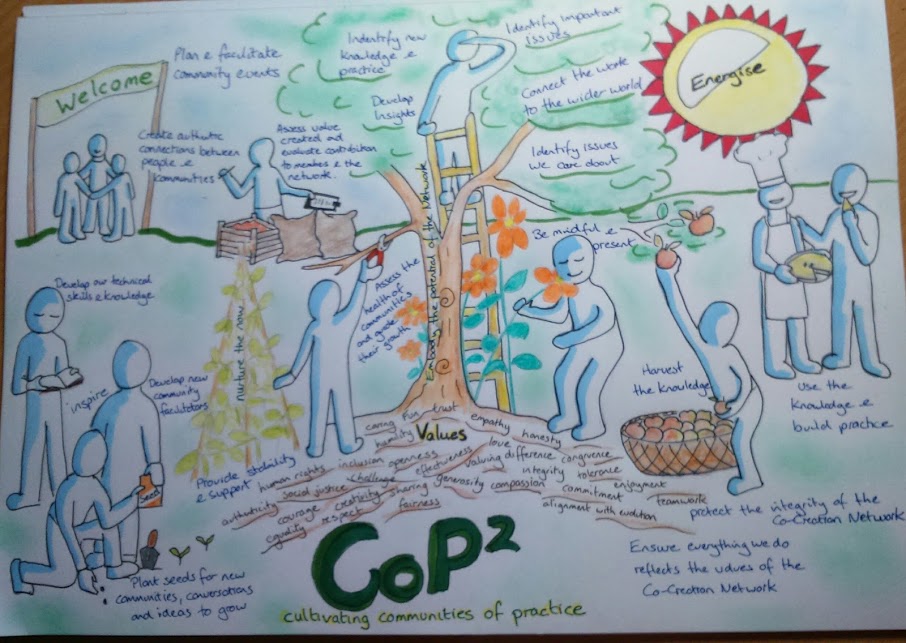
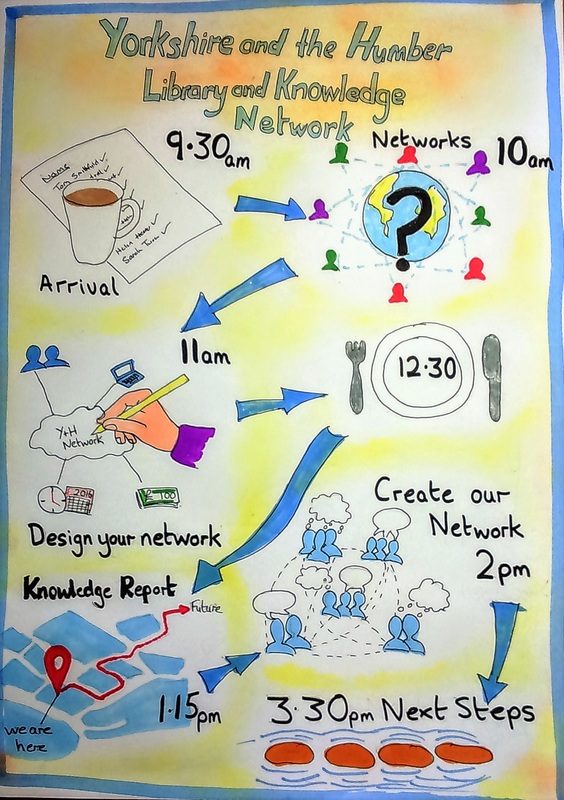
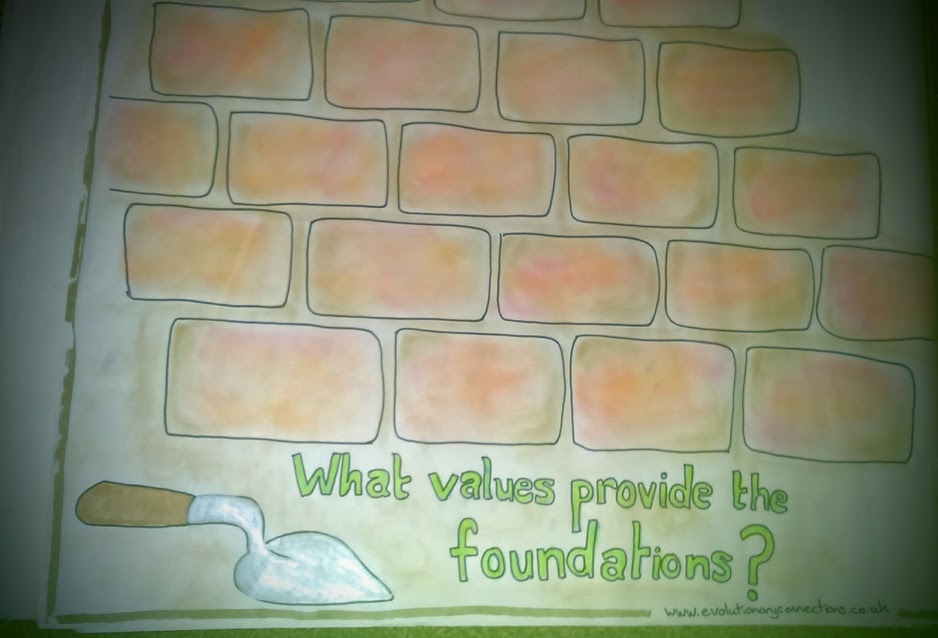
First published Dec 2015  I remember at a meeting, talking to someone working to establish a Teal organisation who told me that the NHS could never be Teal. The NHS is a long way from Teal, for sure. The NHS as a governmental entity is formed of many different organisations. Right now it’s probably more of a rainbow than any particular colour, in terms of the developmental stages of its units. Even so, the NHS and the services it incorporates have made many big changes previously. For example, I was part of the alliance between health and social care staff, families, and service users that worked to move mental health care out of the asylums and into communities. I have worked with some amazing people and I have seen them do incredible things. Maybe they can evolve a Teal NHS; I think so, and this is why. The Current NHS Customarily, particular NHS services have been keen to police and protect their own borders, responsibilities, and resources. In the worst cases, people are bounced between different services, and struggle to find their way in a complex web of providers and eligibility criteria. Sometimes they fall in-between services and their needs go unmet or they just give up. For example, when I was pregnant I had pregnancy-related carpal tunnel and needed a wrist splint. I was told by the physiotherapist I saw at my local primary care clinic that she couldn’t provide it to me, as her budget didn’t cover pregnant women. She advised I should travel into the city to the acute hospital maternity unit and see the physio there. I gave up and bought one via the internet. Institutional Context of the Co-Creation Network of Communities of Practice I have been working for the past year with a group of NHS clinicians, academics, service users, and staff from charitable and private industry to establish what we call the Co-Creation Network which encompasses a variety of “Communities of Practice” committed to making improvements in the health and social care system. The Teal characteristic of evolutionary purpose is evident in that these Communities are about making improvements partly by breaking down the traditional boundaries of health and social care services, and encouraging/implementing a community-encompassing approach. The Network is sponsored by two regional NHS bodies: Yorkshire & Humber Leadership Academy and Yorkshire & Humber Academic Health Science Network. Both regional bodies recognise that the challenges faced by the health and social care system require something very different. Both bodies have struggled to hold the space for this Network and the different approach it takes, against the usual system demands for performance management to justify any investment and direct activity. Communities of Practice are a voluntary, not delegated endeavour. Some participants are given leave to attend meetings and events in worktime, but most CoP activity is done in members’ own time. Thus, membership in a Community of Practice requires great passion and personal motivation. How the Communities of Practice Operate Each CoP is people working together to co-create new knowledge and practice in an aspect of their own field. Communities are varied, focusing on whatever their members see as important. For example, Communities of Practice have been established to consider Sepsis, Medication Safety, and Creating Caring Cultures. The Sepsis CoP is working on awareness-raising techniques to address an issue that people have not been well aware of previously. The NHS system has given them implicit permission by tasking staff or organisations to reduce sepsis incidents, but has not given directives on how to do this. So the CoP has the freedom to develop and implement some “How’s.” You might be wondering, how do new “ways” get authorized to be implemented and put into practice in various settings? In some cases, the system has not given permission (versus the implied permission re Sepsis concerns) and the CoP may be challenging received wisdom and practice. Some CoP’s have been formed with the express intention of doing such challenging, as they strongly believe that current practice is not good enough. CoP’s looking at changing the traditional relationship between professionals and patients are often in this position. Part of their learning is how to identify and influence key stakeholders to co-create a new approach. The Communities of Practice are courageously pursuing new knowledge and new practices that they believe can bring real value to the services they provide. In an acute hospital, a Community of Practice has introduced mindfulness practices for staff and elderly patients. It is reporting a real cultural shift in the ward environment, and a huge impact on patient safety, with fall rates hugely reduced. This Community is now turning its attention to how it might extend this ethos of care out into the community to involve everyone who might provide support to their patients. A Community of Practice was formed by a group of staff developing a new role in primary care to connect services and provide better care for older people with complex health needs. In the UK, locally-based clinics provide access to doctors, nurses and health care support staff as the first point of contact − and principal point of continuing-care contact − for services dealing with ongoing health conditions. It was noted that an older person with several long term conditions such as heart disease, diabetes, and dementia would be in contact with their local primary care doctor and nurses, but would also have links with a huge variety of other health and care organisations including specialist medical services provided at outpatient clinics in acute hospitals, specialist community-based teams such as mental health and dementia care, specialist home care services from a physiotherapist or occupational therapist, nursing visits from charities, as well as support and care workers from not-for-profit care companies. This Community of Practice is noticing early signs of expected success in reduced admissions to hospital for this patient group as all those services work better together to keep the person safe and well at home. There is also a vast array of other benefits from this CoP’s connecting of services. They include improved understanding and appreciation between different government-provided health and social care services, good relationships between different locally-based clinics, authentic connections between statutory (government-provided) services and community assets and resources, and a commitment from all elements of the whole system to improve the support provided to these elderly members of their local community. Next-Stage Challenges Faced and Dealt with in CoP’s I believe my experience provides one bit of clear evidence that the three Teal principles of self-management, evolutionary purpose, and wholeness have been readily adopted as core principles by some NHS staff and those working with them. I am sure there are other examples too. The Communities of Practice established as part of the Co-Creation Network adopted these principles despite the fact that they were challenging and difficult at first. Self-Management Communities of Practice are self-managing by definition. They set their own agenda, organise themselves, and also decide what learning they will pursue and how they will use this knowledge. This was a shock to many NHS staff involved, and it was difficult not to seek permission and direction from elsewhere. Many of us experienced confusion at first. “What is it we are supposed to do?” Communities moved swiftly from confusion to feelings of liberation and then action. Members gained confidence, established relationships, defined their shared agenda, and organised meetings and “learning expeditions” — our title for the work to answer the questions we have set ourselves. Wholeness One of the most unifying and important aspects of the Co-Creation Network is the way it supports wholeness. The Network adopted mindfulness practices to help stressed, overstretched members be fully present in their Communities of Practice. The opportunity to make authentic connections and pursue work that they identified themselves as important was cathartic. I think it may have even persuaded some members, who were disillusioned and damaged by their working environments, to stay within the NHS and work towards change. “This work gave me space to connect with that passion again and start to explore what could be possible. Through learning about CoP’s I could see that I wouldn’t make it to the top (of the mountain) on my own, but I could take others with me and we could support each other on our difficult journey. And that the journey itself would make us stronger, through sharing and learning together.” Community of Practice Member Evolutionary Purpose Perhaps most inspirational is the evolutionary purpose evident in the Network and its Communities of Practice. Free to pursue their own agendas, Communities of Practice have been established to consider pharmacy, mental health and childbirth, work with older people, the role of mindfulness in healthcare, Innovation, Musculoskeletal Practice, and many other areas. However, it’s not the rich variety of learning and practice being developed that I find so significant; it’s the way this is being done, described in this article. Like for Buurtzorg in the Netherlands, the results can already be termed “outrageous”. (Laloux, 2014 Reinventing Organisations, Chapter 2.2 Outrageous Results paragraph 1) “There was an absence or at least a much reduced sense of fear about “doing it wrong;” this felt different from much of my previous experience of the NHS.” Community of Practice Consultant Reinventing the NHS as Teal Contrary to my own typical experience of “falling through the cracks” of the system, now more new Communities of Practice are focusing on working across traditional service boundaries, and often exploring a geographically-defined approach which reflects the community or neighbourhood experience of the people accessing their services. These Communities of Practice seem to have found a real evolutionary purpose. They are working towards breaking down traditional NHS boundaries and developing new ways of supporting health and well-being in an environment where it is clear that health and social care needs to radically reinvent itself. Maybe the person I met was right after all. The NHS as it is now cannot be a Teal organisation. But the NHS that will be, must evolve to become a Teal organisation. previously published Enlivening Edge 27th October 2015 http://www.enliveningedge.org/organizations/uks-national-health-service-nhs-cannot-teal-organisation/#more-1448
I had an unexpected childhood. In the early 1970s my father left his respectable and secure job in a nationalised industry and headed off to university. It wasn’t until I was going through some of his books after he died and came across a passage he had marked about education for education's sake, that I began to appreciate why he had taken this decision. As a student at Ruskin College Oxford, Ruskin’s concept of education as “leading human souls to what is best, and making what is best out of them.” was a core aspect of his motivation to become an educator. In the 1970s it was not done to leave a good job and pursue an uncertain future, especially if you were already in your thirties with a young family to support. I will never know what made him realise that the steady job would not be steady for much longer or what gave him the courage to pursue what was really important to him. I do know that it delivered financial stability and despite its challenges, I think it delivered real job satisfaction too.
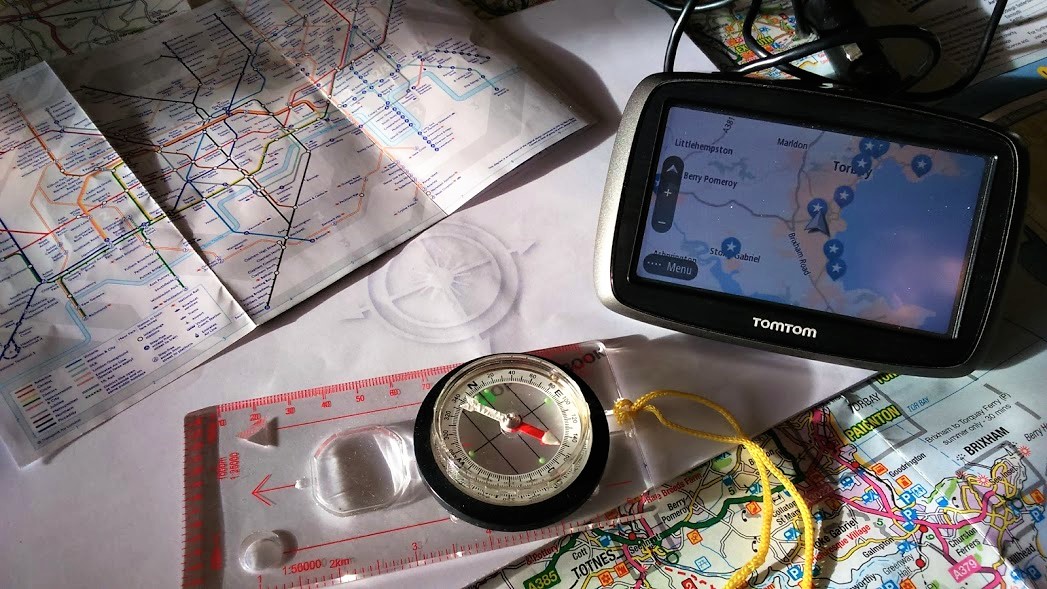
My father’s actions were unusual at the time but now his story seems much more familiar. There are a number of recent pieces of US and UK research recording how most of us will have a number of jobs with an increasing number of employers during our working lives. The Association of Accounting Technicians research in 2015 interviewed 2000 people and found that 46% would change their career completely after finding their current path wasn’t for them. It is much written about that millennials and younger people in the workforce expect much more than a wage packet as fair recompense for their labour. Our relationship with work is more complex and sophisticated than it used to be. Whilst income is important; job satisfaction, well-being, work-life balance, development opportunities and working for an employer that demonstrates social responsibility and where we feel proud to be part of the organisation are also key. It is now recognised that being able to align our personal values and motivations to that of our business or employer is vital to productivity. When we are not fully engaged with our jobs, when we are not convinced our job is worth doing, when we don’t feel we are making the best of our talents, or being enabled to do the best job we can, we are less efficient and the quality of our work suffers. The CMI Quality of Working Life Report 2016 found motivation was becoming an increasing challenge for managers, 28% reported feeling not very motivated or not motivated at all. Over a third of public sector managers reported feeling demotivated and working at less than 70% productivity. More now than ever, it’s important to have a clear understanding of what motivates and drives us and how we can align this in our work to do a job worth doing and do it well. The fast changing world of work and business means that we need to accept that the "what" and "how" of our work will change frequently. We must have a deep understanding of the "why" in order to provide the compass to navigate our future career path and deliver satisfaction, well-being and success. This article was inspired by Lani Morris https://www.greenleaf-publishing.com/the-map-of-meaning |
AuthorJane Pightling has experience across the public, private and charitable sector. Through her work in the NHS Leadership Academy and her consultancy Evolutionary Connections she developed complex systems leadership capacity, providing training, coaching programmes and establishing networks and communities of practice to sustain learning. She maintains her social work registration and her commitment to person centred and community focused approaches. Jane has a deep interest in the potential offered by new ways of working, designing and building organisations and communities that can best deliver this kind of service. She works with organisations and leaders to develop approaches that design in autonomy, wholeness and purpose. Archives
October 2021
Categories
All
|


 RSS Feed
RSS Feed