|
First published 29th January 2019 British Medical Journal
https://blogs.bmj.com/bmj/2019/01/29/jane-pightling-designed-in-the-right-way-social-prescribing-could-deliver-huge-benefits-lets-not-waste-it/?fbclid=IwAR0sgccwjpqV72Bu9E8HfkGwtXwiUUBYvUaz3Wt3egjuwIZgj3xxlXPCFZU
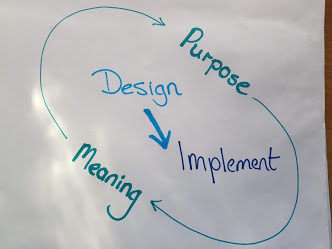
There has been much discussion about social prescribing since funding announcements were made over the summer. Yesterday it was announced that more than 1000 link workers will be recruited by 2020-21 to help with social prescribing. I understand the appeal. I recently worked with a group of GPs who despaired that what they had on offer could not help most of their patients. Many of the people they saw did not need diagnosis or treatment, but access to social opportunities, debt advice, or lifestyle support. Social prescribing can help us feel that we are doing something useful, and it also taps into the prevention agenda. How much more efficient we could be if we prevented illness. However, I have some concerns. Social prescribing is being talked about as a new panacea. I think it could make a difference, but only if we agree its intended purpose and deliberately align our approach to this. Is the aim to reduce demand in GP surgeries to help manage increasing demand? An aging workforce and difficulty recruiting and retaining staff compound capacity issues. GPs aim to provide what their patients need, and they want to make a difference. Some hail social prescribing as a return to the service they used to provide 25 years ago, before the implementation of the 10-minute appointment. Diverting demand to a community marketplace and seeking to reduce future demand in this way could be helpful. But, this aim is about moving demand in the system from one place to another, and does not challenge the system itself. Social prescribing is also described as a lever for change, which aims to redefine medical practice, help GPs embrace a holistic approach, connect with the communities they work within and deliver person-centred care. It has been reported as a radical new way of working. An approach to deliver the prevention agenda thereby reducing demand permanently and creating a sustainable health and care system for the future. These aims are transformational, they intend to change power relationships, beliefs, and attitudes that underpin our practice, and the way we design and deliver services. I believe this initiative does have the potential to deliver transformation. Social prescribing could be a way to build communities and individuals who are health literate, motivated, and resilient enough to promote their own health and wellbeing. However, social prescribing can only deliver this if we act intentionally and align the way that we design and deliver the programme with this purpose. We need to learn lessons from other similar initiatives. The story of Sure Start shows how we can unintentionally destroy social capital in a well-intentioned attempt to improve things. The evaluation showed how Sure Start adversely impacted on existing community provision for young families such as playgroups and how the Sure Start services were used more by families from higher socio-economic groups. I recently spent time with a small community arts project. They told me GPs want to refer to the project, but are unable to. Referrals can only be made to services that have been funded by social prescribing money. The arts project will close soon as their previous funding source has ceased. But there are some positive examples. The “social prescribing” that has been taking place in mental health services for over a decade has much to teach us. Initiatives such as Creative Minds which is run with South West Yorkshire Partnership NHS Foundation Trust have achieved impressive results. The approach that they used gave resources and the power to decide how to deploy them to the people who would use the services. If we ignore this learning and continue to use traditional language, thinking, and tools to implement social prescribing then, we will not deliver transformational results, but perpetuate, and maybe even worsen, the current situation. The words “social prescribing” do not challenge the traditional medical sphere, but reinforce it. Accessing these resources requires a visit to and referral from the GP. As funding is directed to support this scheme, GPs will become gatekeepers to services that people used to access directly. Deprived of funding, the provision people used to attend independently will cease. We may unwittingly increase dependency, rather than promote independence. If we intend to deliver something radical, we must design services in a way that involves GPs in civil society and which can manifest the community’s own definition of health and wellbeing. For communities to promote healthy lives, we need to recognise their strengths, delegate power and resources, and trust and support them to build resilience. To deliver change in the system we will need to change ourselves, our attitudes, the way we work, and our relationship with citizens and communities. Designed in the right way this initiative could deliver huge benefits, let’s not waste it. I responded to Anya De Longh this morning. https://blogs.bmj.com/bmj/2018/10/03/prescribing-personalised-social-pharmacological/
I describe myself as having an allergic reaction to the term social prescribing and this I think my answer below helps to explain why. It’s good that we are starting to recognise health as social and develop our practice accordingly. I worked with a practice recently where GPs were frustrated that what they could provide was not what their patients really needed. It was important to them and to most health care staff to know they can make a difference. Social prescribing enables them to do more of that. I had a conversation yesterday with someone who works for a CIC. They have a 30-year history of working with disengaged and hard to reach groups on community projects which make a difference to the individuals and help build the communities they live in. However, the CIC is under threat as the funding streams from local authorities, youth offending schemes and regeneration have disappeared. He had a conversation with a local GP, aware of the impact of the work the CIC does, who wanted to have this option on his prescribing list. However, a further conversation with the practice manager revealed this was not an option, they could only prescribe to funded projects and social prescribing funds have been cascaded down the health route. By trying to deliver a non-traditional approach in a traditional way we are at risk of further limiting the choice of the people we seek to support. We are viewing the issue through our own “health lens” and allocating resources according to our values and agenda. Activists are receiving the message that if they want to do something in their communities they must fund it themselves or rely totally on volunteers. If we are serious about empowering individuals to take responsibility for their own health and supporting communities to provide opportunities for this to happen then we need to give them the power AND the resources to do this. The issue with social prescribing, which is reflected in the language we use is the power and control. Social prescribing is a good start. I hope that as we change the language of this developing practice we can change the attitudes and the behaviours that underpin it too. We just need to do this quickly or the further community assets that are being starved of resources will wither and die. By Anna Betz and Jane Pightling for Enlivening Edge Magazine Part 1
http://www.enliveningedge.org/views/self-management-save-health-and-care-systems-integral-european-conference/
The role of transformative listening in transforming self and organisations
When both staff and patients have a lot of re-learning to do, we need to develop more advanced skills to listen more deeply to each other, to our own and each others’ values and motivations. We need to learn what it takes to use knowledge wisely to co-create health with individuals and communities. Liberating creative potential encourages the emergence of new insights and practices which is evidenced by the newly formed Wellbeing Teams in the UK. The healing of our broken health and social care systems will require active support of self-care, facilitation of self-knowledge, and working in a highly relational way. This work of healing is inseparable from the way we organise our larger systems of health and care. Courageous and visionary leaders who really care for the system as a whole, and staff who are ready to live their values by working with patients in a way that is empowering, are starting to come together to co-create more dynamic organisational structures. The art of listening is central to this transformative work. Initiatives such as Making Every Contact Count and Shared Decision Making and Health listen to citizens and support them to feel responsible for their own health, and to make lifestyle choices that will enable them to live the life they aspire to lead. This allows them to discover and keep doing what matters to them. If we want to succeed in co-creating healthy systems and health-generating communities, we need to listen from a broader, less outcome-fixated perspective, and create together the conditions that become a fertile soil for the emergence of innovative ideas and practices. Professionals will need to redefine relationships with citizens, and to recognise that we can add value only if we co-produce a solution that recognises the citizen’s strengths, and focuses on what matters to them. Similarly, our organisations need to redefine relationships with our communities. They need to learn to listen without trying to control outcomes, start giving space to communities, and intervene only when invited to help or requested to do things that the community cannot. In this article Anna discussed this aspect in more detail. Jane lives and works in a community that is encouraging staff and citizens to embrace and participate in this new relationship as partners, spending time and resources listening to communities, and developing creative ways to support and provide what the community requests. This has meant developing learning opportunities and coaching for citizens with long-term conditions, co-facilitated by professionals and people with lived experience. It has involved diverting resources to enable citizens to set up groups and networks that meet their own needs. For example, very small resources were required to start an outdoor activity group for dads and children wanting to improve their fitness or to provide a community meeting space for older people with mental health issues to talk and provide each other with support. The setting up of groups and networks included diverting resources to fund a worker to work with homeless people, resisting pressure from the press and local politicians to “remove the problem quickly”. It meant working on the street, listening and waiting until the people themselves decided the time was right to change. It meant supporting the community to come together to develop town centre initiatives to connect existing resources and co-produce and co-implement a plan, securing new resources to provide accommodation and support people back into housing when they are ready. To change the way we have been conditioned by our political, social and educational system to think about healthcare, organise, and deliver it, clearly requires new ways of understanding, designing, and providing it. How can we discover an approach that is energising, revitalising, and enriching, one that builds on strengths and assets within and amongst individuals and communities? It all begins with the quality of our listening and with allowing ourselves to be challenged and transformed by what we sense, hear, and feel called to do and manifest in our lives. Allowing ourselves to be challenged without behaving defensively is connected to a certain quality of thinking or a mindset that we apply when we approach situations. What if the challenges we meet in our life and work are gifts to help us in discovering what else is possible? How can we learn to relate to our own experiences, to each other and to professionals in a way that is empowering and transformational? Otto Scharmer calls the shift in mindset that enables us to connect with more of our human potential a shift in evolving human consciousness from habitual ego-system to eco-system awareness. An eco-system awareness is focusing not only on one’s own wellbeing but on the wellbeing of the whole which broadens the mindset and helps us to listen with more openness. The authors Anna and Jane, along with Helen Sanderson, work in different roles in the health and care sector in the UK. We look forward to sharing with you at the Integral European Conference in May some of our experiences and practices, and we invite you to co-sense and co-discover with us where this journey could take us all. If you are curious about the part you can play in re-inventing health and social care, why not register for the IEC2018 conference and join our two workshops on Friday 25th May? When you register to join the conference following this link don’t forget to mention that you are interested in the Teal Organizations Track.
Join the conversation and help to discover through deep listening what in Christiane Seuhs-Schoeller’s words our “superpowers” are. According to Ria Baeck “most people don’t know and are not aware of what their unique gift to the world is. It is just inside them, totally normal and easy to access.” She has tried to write it in these words: http://www.collectivepresencing.org/6-2-from-authentic-self-to-souls-calling/ To continue the conversation and engage in action together join us at the conference following this linkand remember to mention that you are interested in the Teal Org Track. Part 2 of this article will be published soon. Anna’s background is in Health and Social Care with training in Herbal Medicine, Socialwork, Mindfulness Practice, Transparent Communication, and Systemic Family Therapy. She practices a pro-active evolutionary approach to Health and Wellbeing and leads on projects in the UK National Health Service using Mindfulness and diet for people suffering from chronic inflammatory diseases like diabetes and dementia. Her passion for building thriving and sustainable communities inspired her to co-found the HealthCommonsHub. She feels at home in places where individual, communal, organisational, and social evolution meet, and where people support each other in becoming whole and feel enlivened. |
AuthorJane Pightling has experience across the public, private and charitable sector. Through her work in the NHS Leadership Academy and her consultancy Evolutionary Connections she developed complex systems leadership capacity, providing training, coaching programmes and establishing networks and communities of practice to sustain learning. She maintains her social work registration and her commitment to person centred and community focused approaches. Jane has a deep interest in the potential offered by new ways of working, designing and building organisations and communities that can best deliver this kind of service. She works with organisations and leaders to develop approaches that design in autonomy, wholeness and purpose. Archives
October 2021
Categories
All
|


 RSS Feed
RSS Feed